WINTER 2021 ISSUE
President's Message
Introducing APA's Collaborative Care Model
By Sherin Moideen, MD
PSV President
PSV fall meeting 2021: ‘New Era in Psychiatry’ was held in September at Hilton Norfolk The Main, in downtown Norfolk. The weather was beautiful, and the conference was well attended by members across the Commonwealth, considering that we are still in the midst of the pandemic. PSV Association Managers at Ruggles Corporation worked hard to help conduct the meeting safely. It was a special experience to talk to friends and colleagues in person after a long year of virtual interactions.
We had great guest speakers come from out of town and out of state, as far as Colorado. We learned more about Psychiatry’s past and how it has led us to our current practices so that we can influence the future. We are at a critical point in our history. How psychiatry is practiced is forever changed not only by the impact of COVID-19 on mental health, but also by the accelerated use of digital platforms transforming how we provide medical care. The conference ended with a presentation on ‘Digital Health and the Future of Psychiatry’ and a panel discussion on how we can best utilize technology to address the severe mental healthcare shortage.
This past September, PSV was asked to present at the JCHC subcommittee meeting (General Assembly’s Joint Commission on Health Care). The General Assembly is concerned about the severe behavioral health workforce shortage in the Commonwealth. Solutions and suggestions were presented by a few other disciplines, including psychologists and licensed professional counselors. I represented PSV and spoke about the significant shortage of psychiatrists and noted that the shortage is expected to worsen. It takes several years to train a psychiatrist. Studies have shown that we are not training enough psychiatrists to keep up with the population expansion. Additionally, about 60% of practicing psychiatrists are going to be retiring soon. This is adding to the severe lack of access crisis.
There are 1,907 PGY1 psychiatry residency training slots in the United States, but we only have 41 PGY1 positions in Virginia. Therefore, increasing residency training spots and funding is crucial. We discussed meeting the current and future access crisis by using existing digital platforms to increase our reach and provide quality specialized care. We must ensure that we focus not just on access to care but access to quality care, and that the standard of training and education needs to be maintained. Therefore, I am excited to introduce to you APA’s Collaborative Care Model as a proposed solution for this crisis.
Millions of Americans cannot access quality mental healthcare, and it has been proven that timely and effective preventive care is less costly to healthcare systems, and produces better outcomes. The Collaborative Care Model has a rich body of scientific evidence supporting its effectiveness and affordability. A couple of states have passed legislation supporting collaborative care, and all team members (primary care, behavioral health managers, psychiatrists) and patients are happy with the quality of care, support, and reimbursement.
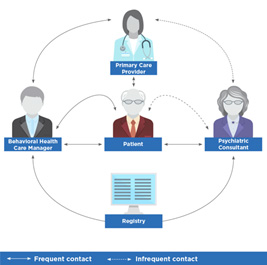 Private practice psychiatrists can easily participate by devoting (adequately reimbursed) one to four hours of clinic time per week to a primary care site. At the top of the model is the primary care physician, who is often the first to hear about mental health concerns, and at the center of the model is a behavioral healthcare manager, who ensures accessibility and works with a psychiatric consultant to provide support (fig: psychiatry.org).
Private practice psychiatrists can easily participate by devoting (adequately reimbursed) one to four hours of clinic time per week to a primary care site. At the top of the model is the primary care physician, who is often the first to hear about mental health concerns, and at the center of the model is a behavioral healthcare manager, who ensures accessibility and works with a psychiatric consultant to provide support (fig: psychiatry.org).
The psychiatrist is often off-site, is consulted by the PCP, and supported by the behavioral healthcare manager who sees the patient more frequently. Psychiatrists can remotely review charts and make expert recommendations focused on preventive care. Psychiatrists can choose to personally evaluate difficult cases before providing a recommendation. The model uses established procedures for assessments and an organized approach to ensure patients receive the most effective care. This model makes quality mental healthcare more accessible to everyone by utilizing telemedicine and integrated care to reach even rural areas. In order to get adequate support to make this model more accessible in Virginia, PSV must work with the General Assembly to introduce legislation similar to other states where this model has been a success. You can learn more about free training and reimbursement models at APA’s psychiatry.org.
This brings me to the last point; we were asked to comment on the reason why many psychiatrists and other behavioral health clinicians are opting out of insurance. We pointed out that one of the main reasons is the mental health parity and ongoing poor reimbursement and high denial rates for behavioral health services. However, several other concerns, including the requirement of excessive documentation (not clinically necessary) and the increased administrative burden on small practices, were also reported by our psychiatrist members in private practice. The JCHC’s own 2020 JLARC report showed that mental health parity is not yet fully achieved in Virginia due to the high denial rate of behavioral health claims. While parity is slowly improving, one of the crucial points necessary to achieve true parity is having an adequate number of expert clinicians in a network. This is still lacking, and it is important to ensure that patients get adequately reimbursed by their insurance companies for seeing an out-of-network psychiatrist, if a network does not have enough psychiatrists. It will also be beneficial to our patients if the process for reimbursement can be a simplified and streamlined process between the insurance company and the client.
Lastly, I am looking forward to seeing everyone in Richmond in February at our 2022 Spring Conference, chaired by our President-Elect Dr. Kara Beatty. The topic is ‘Integrative Psychiatry: Putting it into Practice’. It was amazing to meet colleagues in person after being so limited during the pandemic and we hope to have a great turnout and safely meet again this coming spring. We wish you a happy and healthy holiday season.
Share this content on social media!
JOIN PSV TODAY!
SAVE THE DATES!
PSV 2022 Spring Meeting
Integrative Psychiatry:
Putting it Into Practice
February 25-26, 2022
The Westin Richmond
APA Find a Psychiatrist
Are you accepting new patients?
Opt into APA’s Find A Psychiatrist database. To view the functionality or opt-in,
CLICK HERE
FYI: A link for this option has been added to the PSV website. Select the About button and then Find a Psychiatrist from the drop down.
Letters to the editor and editorial contributions are welcome. Submissions may be sent to Andrew Mann at [email protected]. Paid advertising is accepted on a first come, first served basis. Discounted advertising rates are available to PSV members. To place your advertisement or to request a rate sheet, contact Ray Hall at PSV Headquarters via email at [email protected] or by phone at (804) 565-6313.
© Psychiatric Society of Virginia
2209 Dickens Road | Richmond, VA 23230-2005 | Phone: (804) 565-6377 | Fax: (804) 282-0090 | Email: [email protected] | www.psva.org